Patofisiologi epilepsi erat kaitannya dengan peranan neurotransmiter karena kebanyakan obat antiepilepsi bekerja mengikuti fungsi dari neurotransmiter. Seorang istri mengeluhkan suaminya pada tgl 5 maret 2020 jam 18.00 kejang di rumah 1 x, di mobil 1 x, di IGD 1 x kemudian di beri penanganan, sadar dan. Lebih Lanjut. Tentang Kami.
Abstract
Post‐stroke seizure and post‐stroke epilepsy are common causes of hospital admissions, either as a presenting feature or as a complication after a stroke. They require appropriate management and support in long term. With an increasingly ageing population, and age itself being an independent risk factor for stroke, the incidence and prevalence of post‐stroke seizure and post‐stroke epilepsy is likely to increase. This article examines aetiology, clinical presentation, and presents a management outline of these conditions with particular focus on adults. The aim of this review article is to provide the clinicians with background information and recommendations.
Stroke is the most common cause of seizures in the elderly population., The Oxfordshire community stroke project (OCSP), which examined the immediate and long term risk of seizures after first ever stroke with minimal follow up of two years in stroke survivors, reported that 11.5% of patients with stroke were at risk of developing post‐stroke (that is, delayed) seizures by five years.
In this review article, we use the terms “post‐stroke seizures” and “post‐stroke epilepsy” in the strictest sense. For this article we define post‐stroke seizure as “single or multiple convulsive episode/s (fit/s) after stroke and thought to be related to reversible or irreversible cerebral damage due to stroke regardless of time of onset following the stroke” and post‐stroke epilepsy as “recurrent seizures following stroke with confirmed diagnosis of epilepsy”. As detailed later, early seizures after a stroke will be referred to as post‐stroke seizures rather than post‐stroke epilepsy.
Diagnosis of epilepsy has considerable social and psychological impact on the patients and it should not be made lightly. It has been shown that even in people with mild and well controlled epilepsy, self reported health related quality of life is significantly lower, particularly in social functioning domain of the SF‐36 compared with controls. It seemed that this effect is related to the post‐diagnosis change in their socioeconomic status. The authors also reported mild degree of depression and anxiety, although statistically insignificant, in cases. Post‐stroke epilepsy imposes a clinical dilemma in terms of diagnosis and its management is controversial. Moreover, standard mortality rate, a ratio of the number of deaths found in the patient population, compared with that expected in age and sex matched population, for epilepsy related to cerebrovascular disease, was higher than for all other causes (4.3% and 3.0%). Therefore, a secure diagnosis of epilepsy, treatment tailored to the patient, and continuing integrated care and support are essential.7
Methodology
We performed a literature review in the English language using PubMed/Medline and High Wire Press hosted journal search for the past 25 years (1980 to 2005). We used a two step search strategy at this stage. Firstly, we used the search terms “stroke”, “seizure”, “epilepsy”, and “elderly”. As a second step, we refined our search with the more specific terms of “post‐stroke seizure” and “post‐stroke epilepsy”. We also performed a general search for public domain data using the Google search engine for the key words “epilepsy guidelines”, “National Institute for Clinical Excellence”, “Scottish Intercollegiate Guideline Network”, “American Heart Association”, “Stroke”, and “Epilepsy”.
One author scanned the search results at every stage and selected the most relevant articles and reviews related to the topic. Secondary search was performed using PubMed literature search from the reference list of review articles. Whenever appropriate, related links from PubMed page were checked. We purposely chose the references that were relevant to the areas covered in this review and limited our references list to provide concise and the most relevant information (reading list) to the readers.
Incidence and prevalence of post stroke seizures
Stroke incidence increases with advancing age. Cerebrovascular disease is the number one cause of epilepsy in the elderly population. In a study of unselected population of over 2 million people in England and Wales, Wallace and colleagues found that both age specific incidence and prevalence of epilepsy are higher in older people. The authors reported that the prevalence of epilepsy is as high as nearly 1% in people 85 years and over (6.98–8.66/1000 people).
The OCSP finding that 11.5% of patients with stroke were at risk of developing post‐stroke (delayed or late onset) seizures within five years was very similar to previous population studies. In 1993, Hauser and colleagues reported their Rochester experience both for first seizures and for epilepsy. They studied the incidence of epilepsy and all unprovoked seizures from 1935 through 1984. They found that cerebrovascular disease accounted for 11% of cases. The slope of the accumulative incidence curve increases sharply with age and at older ages the risk of the seizure is higher for men than for women. This is particularly so for the localisation related seizures. By age 75 accumulative incidence of first unprovoked seizures was 4.7% for men and 3.7% for women. Their earlier report showed sharp increases in prevalence of epilepsy for men from 7 per 1000 at 65 years of age, to 15 per 1000 at just over 80 years. The comparative data for women are just over 5 per 1000 and 15 per 1000 respectively.
In a recently reported population based study examining long term outcome of first ever cerebral infarction in 232 young adults, Naess and colleagues reported that 10.5% of them developed post‐stroke seizure over mean follow up of 5.7 years. Hart and colleagues reported recurrence after a first seizure after stroke had recurrent rate of 40% by 12 month in their national general practice study of epilepsy.
Silverman and colleagues highlighted in their recent review that although hospital stroke registry data show that 5%–20% of all people with stroke develop subsequent seizures at some stage, only a subset of this group will develop epilepsy, a condition characterised by recurrent seizures. In an international, multicentre, prospective study based on hospital data involving 2021 consecutive patients with acute stroke, Bladin and colleagues showed the overall incidence of seizures is around 9% during a mean follow up of nine months. Incidence varies with the underlying pathophysiology. Intracerebral haemorrhage is associated with the highest incidence of post‐stroke seizures (10.6%–15.4% of them develop the condition) and transient ischaemic attack is associated with the lowest incidence (3.7%). Some 8.5% of subarachnoid haemorrhages and 6.5% to 8.5% of ischaemic strokes develop this condition.,, Bladin and colleagues also reported that about one third (3% absolute figure) of people with post‐stroke seizure develop recurrent seizures; epilepsy.
This is brought on by an rev.e2 mature driver problem. Dfe-530tx win98 driver for mac.
Classification
The classification of post‐stroke seizure and post‐stroke epilepsy follows a two step process:
The classification of the seizures according to standardised diagnostic (revised) guidelines by the International League Against Epilepsy;
Nosological status of the seizure in relation to the intracerebral event if the seizure occurs within the first two weeks of the stroke onset. Early onset seizures have a peak within 24 hours after the stroke. Around 45% of early onset post‐stroke seizures occur within the first 24 hours. It is described as a late onset seizure, when it occurs after two weeks of stroke onset. Late onset seizure has a peak within 6 to 12 months after the stroke and has a higher recurrence rate of up to 90% in both ischaemic and haemorrhagic stroke., Epilepsy develops in about one third of early onset and half of late onset seizures.
Pathogenesis
There are several causes for early onset seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury (particularly after carotid end arterectomy) have all been postulated as putative neurofunctional aetiologies. Seizures after haemorrhagic strokes are thought to be attributable to irritation caused by products of blood metabolism. The exact pathophysiology is unclear, but an associated ischaemic area secondary to haemorrhage is thought to play a part. Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause. Haemosiderin deposits are thought to cause irritability after a haemorrhagic stroke. In childhood, post‐stroke seizures can occur as part of perinatal birth trauma.
Can we predict who is likely to develop post‐stroke seizures?
It is very difficult to predict who is likely to develop a seizure after the stroke. However, there are some known risk factors associated with a higher incidence of post‐stroke seizures.
In ischaemic strokes; the severity of the initial neurological deficit, the severity of persistent disability after the stroke, the involvement of multiple sites or a larger lesion, cortical damage, and hippocampus involvement are factors that predict the likelihood of developing post‐stroke seizures. Another recognised risk for early post‐stroke seizures is embolic stroke.
However, there is little evidence for intracerebral haemorrhages. In subarachnoid haemorrhages, middle cerebral artery aneurysm, and intraparenchymal haematoma predict the likelihood of post‐stroke seizures. The presence of structural brain lesions, EEG abnormalities, and partial type seizures also carry a higher recurrence rate.
In a hospital based cohort of 1000 Chinese patients, Cheung and colleagues reported that 3.4% of patients included in their study had seizures within one year after stroke. While being male (adjusted OR 3.21) and having a cortical location (adjusted OR 3.83) independently predicted a significantly increased risk, cerebral haemorrhages were shown not to be a risk factor in their study.
Presentation
Post‐stroke seizures typically follow a localisation related (focal) seizure semiology, but about one third of cases present with tonic‐clonic (generalised) seizures and the remaining two thirds usually present with partial seizures. Early onset seizures usually present with a focal onset while generalised tonic‐clonic seizures are more common with late onset seizures. It is worthwhile remembering that there are atypical presentations of post‐stroke seizures as well as seizure mimics; both of which can give rise to confusion and subsequent delay in appropriate diagnosis and management (detailed under Challenges subheading).
Status epilepticus develops in 9% of cases. Although the immediate prognosis of patients with status epilepticus is poor, status epilepticus as a presentation does not predict subsequent development of epilepsy. The independent effect of status epilepticus on mortality outcome is controversial.,, The type of stroke, topographic findings, size of the lesion, or electroencephalographic (EEG) pattern do not predict the progression to status epilepticus.
Role of Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and EEG in diagnosis
When CT is used in conjunction with EEG and clinical findings, it is a useful diagnostic tool to establish the cause of the first seizure in adults. MRI brain is the imaging modality of choice, as it will show a number of abnormalities that may be missed on CT, for example, cortical malformations, hippocampal sclerosis, small mass lesions, and cavernomas—particularly in the temporal lobes.27
EEG can be normal in about 5% of cases and, therefore, normal EEG result does not exclude epileptogenicity. Focal slowing or diffuse slowing activities are associated with a low risk of seizures whereas focal spikes, periodic literalising, or periodic bilateral discharges are associated with a higher risk. In a prospective study with mean follow up of 15.9 months, no specific EEG pattern was found in those who later developed epilepsy.
OverviewStudents who are beginning studies in technology need a strong foundation in the basics before moving on to more advanced technology courses and certification programs. Software Development Fundamentals - 40361 Course Outline (3 days)Voucher NoticePlease note, this class is not eligible for payment through Software Assurance Training Vouchers funded by Microsoft. Microsoft software development fundamentals.
Management
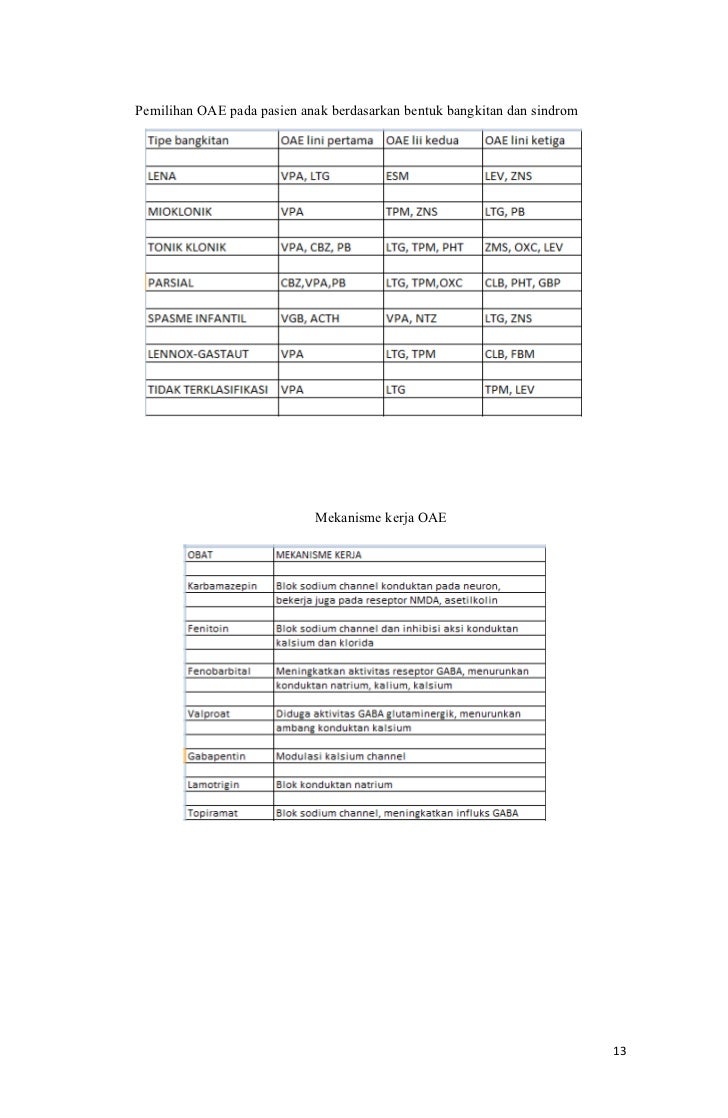
Antiepileptic drugs (AED) remain the mainstay of epilepsy management in all age groups.,30 Single therapy controls the seizures (in 88% of cases). For both focal (with or without generalised tonic‐clonic) seizures and generalised seizures, the recommended first line AEDs include carbamazepine, lamotrigine, sodium valproate, and toppiramate.30 For carbamazepine there has been shown to be a good correlation between the dose and the plasma concentration. Alternative monotherapy includes phenytoin, Phenobarbital, and clonazepam. Phenytoin is the most commonly used alternative, particularly in older patients. The main limitations for all these AED revolve around an associated sedation. Table 11 summarises the advantages, side effects, and recommendations for commonly used AED.
| Drug | Recommended seizure type | Pharmacokinetics | Common side effects | Plasma therapeutic ranges |
|---|---|---|---|---|
| Carbamazepine | Focal/generalised (1° or 2°) | Enzyme inducer | rash, diplopia, headache dizziness, conduction block | 20–50 μmol/l (optimal) |
| Sodium valproate | Any | No enzyme induction | Tremor, weight gain | – |
| Lamotrigene | Except myoclonic | No enzyme induction | Rash | – |
| Phenytoin | Generalised tonic‐clonic and tonic | Enzyme inducer | Gum hypertrophy | 40–80 μmol/l (trough) |
| Megaloblastic anaemia | ||||
| Toxic symptoms and signs— ataxia, nystagmus, sedation dysarthria, diplopia |
Other special considerations of AED use in older population are the possibility of drug interaction because of hepatic enzyme induction by commonly used AED such as carbamazepine and phenytoin, the higher chance of toxic effects because of the pharmacokinetic and pharmacodynamic changes associated with ageing. Drug compliance can also be an issue in older patients.

The Stroke Council of American Heart Association recommends seizure prophylactic treatment in the acute phase for intracerebral and subarachniod haemorrhages. Patients with seizure activity more than two weeks after presentation have a higher risk of recurrence and require long term anticonvulsant prophylactic therapy. Patients with cerebellar or deep subcortical lesions are less likely to develop recurrent seizures and treatment is not recommended routinely. Pragmatically, early onset seizures need treatment for one month and drug treatment can be stopped if no seizure activity occurred during treatment. This is mainly based on a report from Cervoni and colleagues that reported the observed development of epilepsy frequently in the cases of patients affected by late seizures. In a recently published review on epilepsy prophylaxis by Grisar and colleagues, the authors highlighted that in many circumstances AED are used in patients who have never presented any clinical seizures and they are given on the assumption of a potential risk of developing acute or delayed chronic seizures after brain injuries such as trauma, stroke, haemorrhages, or even neurosurgical interventions. They acknowledged the absence of any coherent antiepileptic prophylactic behaviour for delayed/ post‐lesional (unprovoked) epilepsy.
The general principles of management used for epilepsy of any cause also apply to the management of post‐stroke seizures and post‐stroke epilepsy. These include informing the driving licence agency (for example, the DVLA in UK) where people hold a current driving licence, advice on supervision of activities such as swimming, cooking, etc, gradual increment of dose regimen to maintenance dose, and regular follow up for monitoring of drug side effects.
Key points
Seizure and epilepsy after stroke is common.
Late onset seizure has a higher recurrent rate compared with early onset seizure after a stroke.
Atypical seizure forms can occur, particularly in the older people, and a high index of suspicion is required for the correct and early diagnosis of post‐stroke seizure.
Diagnosis of post‐stroke epilepsy has considerable social and psychological impact on the patient and a multidisciplinary team approach, therefore, is essential in its management.
Surgical treatment of intractable epilepsy after ischaemic cerebral vascular events has been considered a valuable means of controlling seizures, but less considered as potential therapeutic intervention. This may have something to do with the population affected in terms of vulnerabilities in relation to their age. This has been seen by Kilpatrick et al and re‐emphasised in a comprehensive review by Kortilla and Wiltimo.
Challenges; It is not always black and white
It is not always clear cut whether the patient has had seizures. Clinically, one can come across a variety of atypical seizure forms particularly in the older people. Acute confusional state, slowing, behavioural change, and syncope of unknown origin are a few of the symptoms post‐stroke seizure can present with. Symptoms also frequently lead to a mistaken diagnosis of stroke recurrence, when the patient is actually experiencing post‐ictal paresis or Todd's paralysis. Godfrey and colleagues (1982) described Todd's palsy, which could last up to four days. The authors also described ictal and post‐ictal confusional states of up to seven to eight days.
Key references
Bladin CF, Alexandrov AV, Bellavance A, et al. Seizures after stroke. A prospective multicenter study. Arch Neurol 2000;57:1617–22.
Silverman IE, Restrepo L, Mathews GC. Poststroke seizures. Arch Neurol 2002;59:195–201.
Broderick J, Adams H Jr, Barsen W, et al. Guidelines for the management of spontaneous intracerebral haemorrhage: a statement for the health care professionals from the special writing group of the Stroke Council, American Heart Association. Stroke 1999;30:905–15.
International League Against Epilepsy. Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepia 1989;30:389–99.
The Royal College of Physicians of Edinburgh. Better care for children and adults with epilepsy—a consensus conference. J R Coll Physicians Edinb 2003;33:2–3.
Another important issue particularly in older adults is distinguishing a post‐stroke seizure from other causes of seizures and from other conditions that can mimic seizures. The most important differential diagnosis is syncope as it can be associated with incontinence, injury, and a slower recovery with confusion, which all are features of seizures. The apparent cause of seizure (that is, stroke) may mask the actual cause of seizure such as neurological (cerebral infections), metabolic (electrolyte imbalance), and cardiovascular (cardiac rhythm disturbances); therefore these conditions need to be considered as differential diagnoses.
Furthermore, the relation between seizures and stroke is quite complex. Shinton and colleagues reported that in patients with acute stroke, seizures might be a harbinger of stroke. Cleary and colleagues recently reported their findings from age, sex, and general practice matched 4709 people with an onset of seizures after the age of 60 years and 4709 controls in terms of stroke risk. They reported almost tripling risk of stroke in cases compared with controls (point estimate relative hazards ratio of 2.89).
Multidisciplinary approach
The diagnosis of epilepsy has a significant impact on the person as well as their families/carers. Education and counselling, directed both at the patient and their families/carers should, therefore, be started in parallel with pharmacotherapy.40 A multidisciplinary team approach is required; epilepsy specialist nurses play a vital part in education, counselling, and reassurance. It may also be helpful to provide relevant contact addresses and help lines. Patient interest groups such as the British Epilepsy Association (BEA) in the UK can play an important part in supporting the patient and their family.
Prognosis
The effect of post‐stroke seizures on stroke outcome remains unclear. While some studies showed better outcome, some reported a worse outcome. In one series, seizures were associated with better outcome in terms of the Scandinavian stroke scales (SSS). In their study, the authors examined the outcome after early seizures in 1197 acute stroke patients. Early seizures were not associated with inpatient death (p = 0.56) but were related to a better outcome, equivalent to increased SSS score of 5.7 points (SE (β) = 1.8; p = 0.002). In another series, authors reported that people who developed early seizures (within 48 hours) after stroke or transient ischaemic attack had higher inpatient death rate (37.9%) compared with who did not present with seizures (14.4%)(p<0.0005). Mortality and morbidity of stroke outcome itself seem to depend on the underlying cause.
Comment
To date, many population and hospital based studies have been performed examining the epidemiology, pharmacological management, and overall outcome (for example, mortality) of post‐stroke seizures and post‐stroke epilepsy. Future research should focus on their impact on stroke outcome, appropriateness, and timing of starting anticonvulsant therapy and the duration of treatment. Moreover, age specific outcome data and the effect of different strategies for its management (for example, community based compared with hospital based), and specific health related quality of life and health utility index measures relevant to post‐stroke epilepsy are also required for a better understanding and optimal management of this common clinical condition.
Contributors
All authors contributed in writing of this article.
Footnotes
References